Innovation in health services is reshaping how we approach healthcare, moving beyond traditional models to embrace cutting-edge technology and patient-centric approaches. From AI-powered diagnostics to telehealth revolutionizing access, the sector is undergoing a dramatic transformation, impacting everything from treatment effectiveness to administrative efficiency. This exploration delves into the key drivers and challenges of this evolution, showcasing how technological advancements, process improvements, and a focus on patient experience are creating a healthier future.
We’ll examine the role of artificial intelligence in enhancing diagnostic accuracy, the transformative potential of telehealth in bridging geographical barriers to care, and the ethical considerations surrounding the use of patient data. We’ll also investigate how streamlined administrative processes, data analytics, and lean management principles are optimizing hospital operations and improving patient safety. The journey will uncover how patient-centered care models, personalized medicine, and blockchain technology are shaping the future of healthcare, leading to more effective, efficient, and equitable care for all.
Defining Innovation in Health Services
Innovation in health services is the process of translating new ideas, technologies, and approaches into improved healthcare delivery, ultimately enhancing patient outcomes and the overall efficiency of the system. This encompasses a wide spectrum of activities, from small, incremental improvements to entirely new models of care. Understanding the nuances of this process is crucial for driving progress in a sector constantly grappling with evolving needs and technological advancements.Innovation in healthcare can be categorized as incremental or radical.
Incremental innovations represent small, iterative improvements to existing practices or technologies. For example, refining a surgical technique to reduce recovery time or developing a more user-friendly electronic health record system are examples of incremental innovation. In contrast, radical innovations represent fundamental shifts in how healthcare is delivered or the underlying technologies used. The development of telemedicine platforms enabling remote consultations or the introduction of CRISPR-Cas9 gene editing technology for disease treatment represent radical innovations.
Incremental versus Radical Innovations in Healthcare
Incremental innovations often involve optimizing existing processes or products. They are generally less risky and easier to implement than radical innovations, often requiring less upfront investment and disruption to existing workflows. However, their impact may be less transformative. Radical innovations, on the other hand, involve significant changes to existing practices or the introduction of entirely new technologies. While they have the potential for greater impact, they are typically more expensive, riskier, and require significant organizational change management.
For example, the introduction of minimally invasive surgical techniques represents incremental innovation, while the development of artificial intelligence-driven diagnostic tools represents a radical shift.
Drivers and Barriers to Innovation in Healthcare
Several factors drive innovation in the healthcare sector. These include the increasing prevalence of chronic diseases demanding new treatment approaches, advancements in medical technology creating new possibilities, the rising cost of healthcare prompting the need for efficiency improvements, and the growing demand for patient-centered care. However, significant barriers also hinder innovation. These include regulatory hurdles and lengthy approval processes for new technologies and treatments, a lack of funding for research and development, resistance to change among healthcare professionals, and concerns about data privacy and security in the context of digital health innovations.
Models of Innovation Adoption in Healthcare Organizations
Healthcare organizations adopt innovations through various models. The diffusion of innovations theory, for example, describes how new ideas spread through a population. This model highlights the importance of early adopters in driving wider adoption. Other models focus on organizational factors such as leadership support, resource allocation, and the creation of a culture that embraces change. Successful adoption often requires a multi-faceted approach, involving effective communication, training, and ongoing support for staff, as well as mechanisms to track and measure the impact of the innovation.
The successful implementation of electronic health records, for instance, requires not only the technological infrastructure but also extensive staff training and ongoing support. Conversely, the failure to adequately address these factors can lead to low adoption rates and ultimately, a failure to realize the potential benefits of the innovation.
Technological Advancements in Healthcare
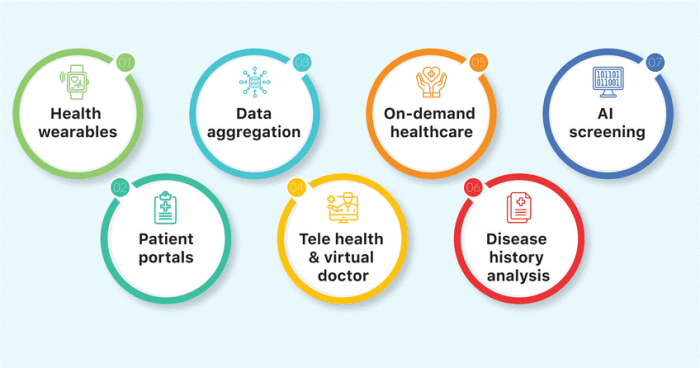
The healthcare landscape is undergoing a dramatic transformation, fueled by rapid technological advancements. These innovations are not only improving the quality of care but also increasing accessibility and efficiency across the board. From artificial intelligence revolutionizing diagnostics to telehealth bridging geographical divides, the impact is profound and far-reaching. This section delves into some key technological advancements shaping the future of health services.
Innovation in health services is rapidly transforming patient care, demanding efficient management systems. Streamlining operations is key, and this is where implementing a robust system like erp online can make a significant difference. Such integrated platforms offer better resource allocation, ultimately leading to improved healthcare delivery and enhanced patient outcomes, further fueling innovation within the sector.
Artificial Intelligence in Diagnostics and Treatment Planning
Artificial intelligence (AI) is rapidly changing the way healthcare professionals approach diagnosis and treatment planning. AI algorithms, trained on massive datasets of medical images and patient records, can analyze information with remarkable speed and accuracy, often surpassing human capabilities in certain areas. For example, AI-powered systems can detect subtle anomalies in medical scans like X-rays and MRIs, potentially leading to earlier and more accurate diagnoses of conditions like cancer and heart disease.
In treatment planning, AI can assist in personalized medicine by analyzing a patient’s unique genetic profile, lifestyle factors, and medical history to recommend the most effective treatment strategy. This precision medicine approach promises to improve treatment outcomes and reduce adverse effects. The use of AI in robotic surgery is also gaining traction, allowing for minimally invasive procedures with greater precision and control.
Telehealth and Improved Access to Care
Telehealth, encompassing remote patient monitoring, virtual consultations, and remote diagnostics, is revolutionizing access to healthcare, especially in underserved and remote areas. Patients in rural communities or those with limited mobility can now access specialists and receive timely medical attention without the need for extensive travel. Telehealth platforms offer a range of services, including virtual check-ups, medication management, and mental health counseling.
This increased accessibility leads to better health outcomes, reduces healthcare disparities, and improves patient satisfaction. However, it’s crucial to acknowledge the challenges associated with telehealth, including issues related to digital literacy, internet access, and regulatory hurdles.
| Feature | Telehealth | Traditional In-Person Care |
|---|---|---|
| Accessibility | Improved access for remote patients and those with mobility issues. | Limited by geographical location and patient mobility. |
| Cost-Effectiveness | Potentially lower costs for both patients and healthcare providers, reducing travel and time expenses. | Higher costs associated with travel, waiting times, and in-person consultations. |
| Convenience | Increased convenience and flexibility for patients, scheduling appointments at their convenience. | Requires travel and adherence to fixed appointment times. |
| Limitations | Requires reliable internet access and technological literacy; may lack the physical examination component crucial for some diagnoses. | Limited by availability of healthcare professionals and appointment scheduling. |
Wearable Technology for Preventative Healthcare and Personalized Medicine
Wearable technology, such as smartwatches and fitness trackers, offers exciting possibilities for preventative healthcare and personalized medicine. Imagine a scenario where a patient with a family history of heart disease wears a smartwatch that continuously monitors their heart rate, blood pressure, and activity levels. If the device detects an abnormal heart rhythm or other concerning patterns, it automatically alerts the patient and their physician, allowing for prompt intervention and preventing a potential cardiac event.
This proactive approach to healthcare shifts the focus from reactive treatment to preventative care. Furthermore, data collected from wearable devices can be used to personalize treatment plans. For instance, a diabetic patient’s insulin dosage can be adjusted based on real-time glucose readings from a continuous glucose monitor (CGM), ensuring optimal blood sugar control and minimizing the risk of complications.
This personalized approach to healthcare leverages technology to empower individuals to take control of their health and improve their overall well-being.
Improving Healthcare Processes and Efficiency
Streamlining healthcare processes is crucial for improving patient outcomes, reducing costs, and enhancing the overall quality of care. Innovation plays a pivotal role in achieving this, focusing on optimizing administrative tasks, leveraging data for better decision-making, and implementing efficient management strategies. This section explores several key areas where innovation is transforming healthcare efficiency.
Innovative Approaches to Streamlining Administrative Processes
Hospitals often grapple with complex administrative tasks, consuming significant time and resources. Innovative approaches are crucial for reducing administrative burden and freeing up staff to focus on patient care. Three notable strategies include implementing electronic health records (EHRs) effectively, leveraging robotic process automation (RPA), and adopting cloud-based solutions for data storage and management.
- Electronic Health Records (EHRs): While EHRs are not new, their effective implementation remains a key area for improvement. Optimized EHR systems can automate tasks such as appointment scheduling, prescription refills, and billing, reducing manual paperwork and improving data accuracy. Successful implementation requires robust training for staff, integration with other hospital systems, and a focus on user-friendliness to minimize frustration and ensure adoption.
- Robotic Process Automation (RPA): RPA involves using software robots to automate repetitive administrative tasks, such as data entry, claims processing, and appointment reminders. This technology can significantly reduce manual workload, minimize human error, and free up staff for more complex and patient-focused tasks. For example, RPA can automate the process of verifying insurance coverage, reducing the time spent on manual checks and improving efficiency.
- Cloud-Based Solutions: Migrating to cloud-based systems offers significant advantages in terms of data storage, accessibility, and scalability. Cloud solutions provide secure and centralized access to patient information, facilitating collaboration among healthcare providers and reducing the risk of data loss. This also allows for easier data analysis and reporting, leading to better informed decision-making.
Utilizing Data Analytics for Enhanced Patient Safety and Error Reduction
Data analytics offers powerful tools for improving patient safety and reducing medical errors. By analyzing large datasets of patient information, hospitals can identify trends, predict risks, and implement proactive interventions. This involves the use of predictive modeling, real-time monitoring, and anomaly detection.
For instance, analyzing patient data can identify individuals at high risk of developing hospital-acquired infections (HAIs). Predictive models can flag these patients, allowing healthcare providers to implement preventative measures such as enhanced hygiene protocols or prophylactic antibiotics. Similarly, analyzing data on medication errors can highlight patterns and identify areas where processes need improvement, leading to the implementation of safety checks and protocols to prevent future errors.
Real-time monitoring of vital signs and other patient data can also alert healthcare professionals to potential problems, allowing for prompt intervention and improved patient outcomes. Anomaly detection systems can identify unusual patterns in patient data that might indicate a developing complication, enabling early diagnosis and treatment.
Lean Management in Healthcare: A Case Study
Lean management principles, originally developed in manufacturing, have been successfully adapted to healthcare settings to improve efficiency and reduce waste. A notable example is the implementation of lean principles at the Virginia Mason Medical Center in Seattle. They focused on eliminating unnecessary steps in processes, reducing waiting times, and improving workflow.
Virginia Mason implemented a comprehensive lean transformation program, involving all levels of staff. They used tools such as value stream mapping to identify bottlenecks and areas for improvement in their processes. This resulted in significant reductions in patient wait times, improved surgical efficiency, and a decrease in medication errors. The program also fostered a culture of continuous improvement, empowering staff to identify and implement process improvements.
The success of Virginia Mason’s lean transformation demonstrates the potential for improving healthcare efficiency through the systematic application of lean principles. Key elements included a strong commitment from leadership, staff involvement in process improvement initiatives, and the use of data to track progress and measure success.
Patient-Centered Innovation
The healthcare landscape is undergoing a dramatic shift, moving away from a provider-centric model to one that prioritizes the individual patient’s needs and preferences. Patient-centered innovation is at the heart of this transformation, recognizing that effective healthcare isn’t just about delivering treatments; it’s about empowering patients to actively participate in their own care and achieving the best possible health outcomes.
This approach necessitates a fundamental change in how healthcare is delivered, emphasizing shared decision-making, personalized care plans, and a holistic understanding of the patient’s life.Patient-centered care models prioritize individual preferences and values when making treatment decisions. This means going beyond simply providing information and actively engaging patients in a collaborative dialogue to determine the best course of action. It involves understanding a patient’s personal goals, their understanding of their condition, and their tolerance for different treatment options.
For instance, a patient facing a complex surgery might prioritize a quicker recovery time over a slightly lower risk of complications, a preference that should be carefully considered and incorporated into the treatment plan. This shared decision-making process fosters trust and ensures that the chosen treatment aligns with the patient’s overall well-being and priorities.
Shared Decision-Making and Personalized Care Plans
A key component of patient-centered care is the implementation of shared decision-making. This involves a collaborative discussion between the healthcare provider and the patient, where both parties contribute to the decision-making process. This contrasts with the traditional model where the provider dictates the treatment plan. Shared decision-making requires the provider to present clear, unbiased information about different treatment options, including their benefits, risks, and potential side effects, allowing the patient to make an informed choice that reflects their values and preferences.
This approach is particularly important for patients with chronic conditions requiring long-term management, where patient adherence to the treatment plan is crucial for successful outcomes. Personalized care plans, tailored to the individual patient’s needs and preferences, are a direct outcome of this collaborative process.
Patient Engagement and Improved Health Outcomes
Active patient engagement significantly improves health outcomes and reduces healthcare costs. When patients are actively involved in managing their health, they are more likely to adhere to treatment plans, leading to better disease control and reduced hospital readmissions. For example, patients with diabetes who actively participate in self-management programs, including regular blood glucose monitoring and lifestyle modifications, tend to experience better glycemic control and fewer complications.
Furthermore, patient engagement can lead to more efficient use of healthcare resources. Patients who are well-informed and actively involved in their care are less likely to seek unnecessary medical attention, reducing overall healthcare costs. This proactive approach empowers patients to become active participants in their healthcare journey, resulting in better health outcomes and reduced strain on the healthcare system.
Ethical Implications of Using Patient Data, Innovation in health services
The use of patient data for research and innovation presents significant ethical considerations. While the potential benefits of using patient data to develop new treatments and improve healthcare delivery are undeniable, it is crucial to ensure that this data is used responsibly and ethically. This requires robust data protection measures, including anonymization and encryption, to safeguard patient privacy.
Informed consent is paramount, meaning patients must be fully informed about how their data will be used and have the right to withdraw their consent at any time. Transparency in data usage and clear guidelines on data sharing are essential to build trust and maintain public confidence in the use of patient data for research and innovation. Striking a balance between the potential benefits of data-driven innovation and the need to protect patient privacy is a crucial ethical challenge that requires ongoing attention and careful consideration.
The Future of Innovation in Health Services

The healthcare landscape is poised for a dramatic transformation, driven by converging technological advancements and a growing emphasis on personalized and preventative care. Emerging trends are rapidly reshaping how we diagnose, treat, and manage health, promising a future where healthcare is more effective, accessible, and patient-centric than ever before. This section explores some of the key innovations driving this evolution.
Personalized Medicine and Gene Therapy
Personalized medicine represents a paradigm shift, moving away from a “one-size-fits-all” approach to treatment towards tailored therapies based on an individual’s unique genetic makeup, lifestyle, and environmental factors. This approach leverages advancements in genomics and data analytics to identify specific genetic markers associated with disease susceptibility and response to treatment. For instance, genetic testing can now predict an individual’s risk for certain cancers, allowing for proactive screening and preventative measures.
Gene therapy, a closely related field, goes a step further by directly modifying a person’s genes to treat or prevent disease. This technique holds immense potential for treating currently incurable conditions like cystic fibrosis and certain types of cancer. While still in its early stages, gene therapy has already shown remarkable success in clinical trials, paving the way for future breakthroughs.
Imagine a future where genetic predispositions to diseases are identified early, enabling personalized preventative strategies and targeted therapies, dramatically improving health outcomes.
Blockchain Technology in Healthcare
Blockchain technology, known for its secure and transparent nature, offers significant potential for improving data security and interoperability in healthcare. The decentralized and encrypted nature of blockchain makes it highly resistant to hacking and data breaches, a critical concern in the healthcare industry where sensitive patient information is constantly being shared. By creating a secure and auditable record of patient data, blockchain can enhance trust and transparency across the healthcare ecosystem.
Furthermore, blockchain can facilitate seamless data exchange between different healthcare providers, eliminating data silos and improving care coordination. For example, a patient’s medical history could be securely stored on a blockchain, accessible to authorized healthcare providers across different systems, enabling a more holistic and informed approach to patient care. This improved data sharing would lead to better-coordinated care, reduced medical errors, and improved patient outcomes.
Design Thinking in Healthcare Innovation
Design thinking, a human-centered problem-solving approach, is increasingly being applied to develop innovative solutions to healthcare challenges. This iterative process emphasizes empathy, experimentation, and collaboration to create solutions that are both effective and user-friendly. By focusing on the needs and experiences of patients and healthcare providers, design thinking can lead to the development of more intuitive and accessible healthcare products and services.
For example, design thinking principles have been used to create more user-friendly medical devices, improve the patient experience in hospitals, and develop innovative solutions for managing chronic diseases. A hospital using design thinking might redesign its waiting rooms to be more comfortable and less stressful for patients, or a medical device company might develop a simpler, more intuitive insulin pump.
This human-centered approach ensures that innovations are not only technologically advanced but also address the real-world needs of those they are intended to serve.
Illustrative Examples of Innovation: Innovation In Health Services
Innovation in healthcare isn’t just about futuristic gadgets; it’s about tangible improvements impacting patients and the system as a whole. Let’s explore some compelling examples that showcase the transformative power of innovative approaches.
A Novel Diagnostic Tool Workflow
Imagine a visual representation of a new diagnostic tool’s workflow. The layout is a circular flow chart, starting at the top with a bright teal circle representing “Sample Collection.” Arrows, a vibrant orange, lead to a dark green hexagon depicting “Automated Sample Preparation.” This hexagon connects to a central, large, light purple square representing “AI-Powered Analysis,” which is the core innovative aspect.
From this square, another set of orange arrows points to a light blue oval labeled “Results Reporting,” which then leads back to the teal circle, completing the cycle. The overall design emphasizes the seamless integration of automation and AI, highlighting the speed and accuracy of the new tool compared to traditional methods. The AI-powered analysis section is noticeably larger to visually emphasize its crucial role.
Impact of Innovative Intervention on a Patient’s Health Journey
Consider a patient, Sarah, diagnosed with Type 2 diabetes. Traditional management involved frequent blood tests, multiple medications, and strict dietary restrictions. However, a new personalized medicine approach, using genetic analysis and AI-powered predictive modeling, significantly altered her journey. This innovative intervention identified her specific genetic predisposition to insulin resistance and tailored a medication regimen and dietary plan precisely to her needs.
The result? Sarah experienced improved blood sugar control, reduced medication side effects, and increased energy levels. This personalized approach reduced her hospital visits and improved her overall quality of life, showcasing the profound impact of precision medicine. Her improved adherence to the treatment plan, due to its personalized nature, further exemplifies the success of this innovative intervention.
Socio-Economic Implications of a Major Technological Advancement
The widespread adoption of telehealth technology during the COVID-19 pandemic presents a compelling case study. While initially driven by necessity, telehealth demonstrated significant socio-economic benefits. Reduced travel costs for patients, particularly those in rural areas or with mobility issues, led to improved access to care. Simultaneously, healthcare providers saw increased efficiency and reduced overhead costs. However, the digital divide highlighted the need for equitable access to technology and internet connectivity, revealing a potential barrier to the widespread and fair adoption of this technology.
The increased demand for skilled telehealth professionals also impacted the job market, creating new opportunities while potentially displacing some traditional roles. This complex interplay of benefits and challenges underscores the need for careful planning and policy adjustments to maximize the positive socio-economic impact of such advancements.